Member Services Information
The Vault Health Plan is owned by its participants but is administered by Vault Administrative Services. Vault Admin Services ensures you receive fair pricing for your health services and prompt payment to your healthcare providers.

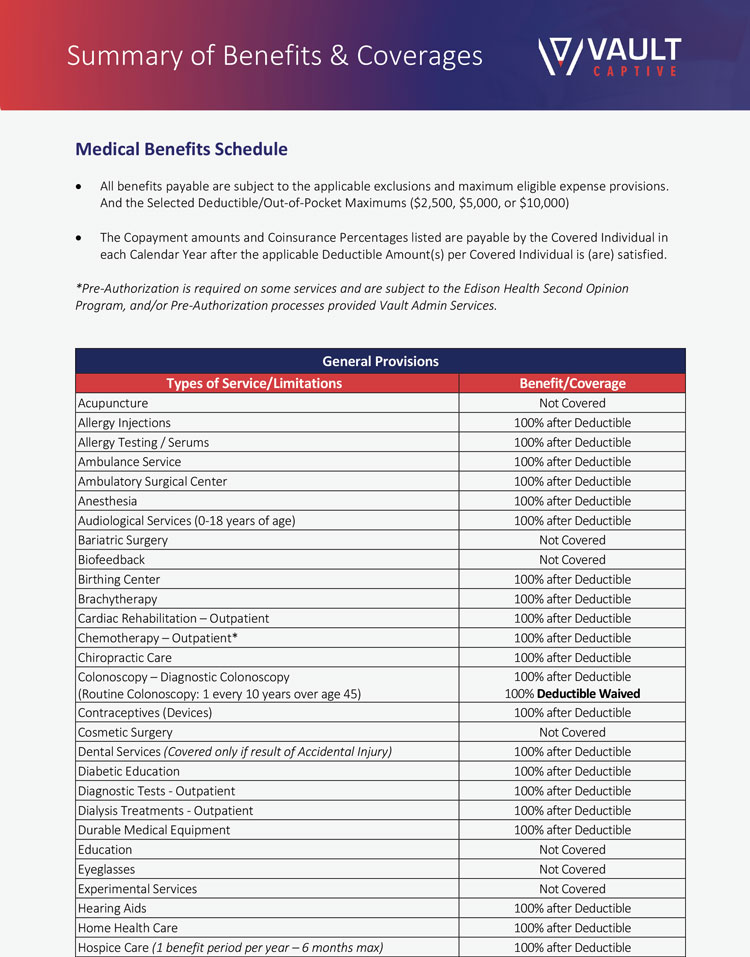
For Eligibility, ID Cards, Verification of Benefits, Medical Claims and Pre-Authorization:
Vault Admin Services: 866-202-0029

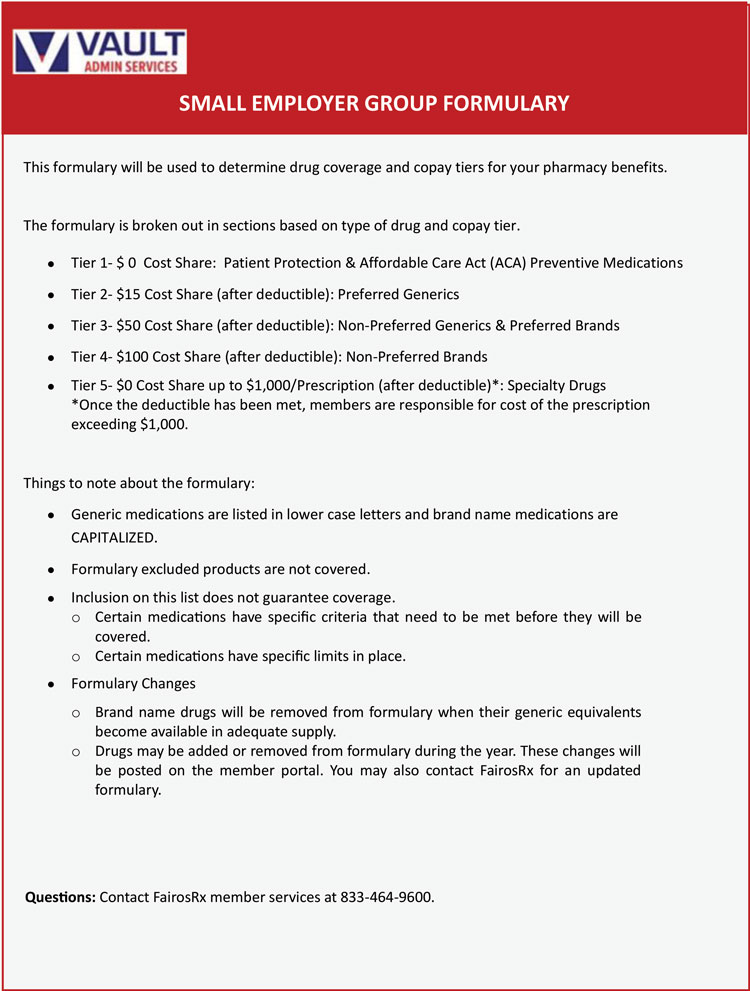
Pharmacy Helpdesk:
833-464-9600
Questions regarding your pharmacy benefits?

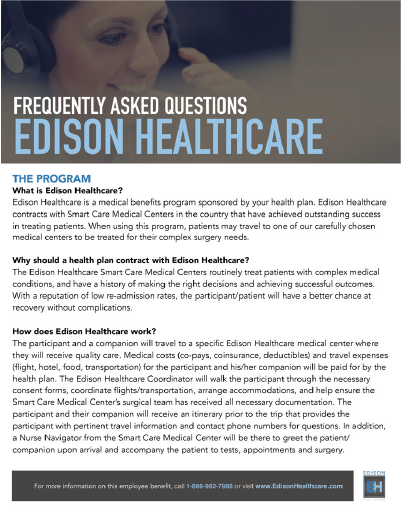
866-982-7988
edisonhealthcare.com
Looking to schedule a surgery or specialized medical treatment?
Member Resources: Frequently Asked Questions (FAQs)
Present your ABC Health Benefits card—just like any other health insurance plan you’ve used. You do not pay at the time of service.
Yes, of course! The best course of action is to call your provider to make the appointment, then call Vault Admin Services to verify the benefits prior to the appointment, then be sure to take your card to your provider on your appointment day. And if you forget to call ahead of time to verify your benefits, that’s okay too.
Your healthcare provider should call 866-202-0029 (located on the back of your card) to validate and file using the information on the back of the card. A few weeks after your health service, you will receive an Explanation of Benefits (EOB) You are only responsible for the amount designated as ‘patient responsibility’ on the EOB.
If the provider bill states you owe more than the balance shown as ‘patient responsibility’ on the EOB, this is a ‘balance bill.’ Call Vault Admin Services immediately at 866-202-0029. A patient advocate will answer your questions and determine whether a dispute should be filed. Be sure to do this within 60 days of receiving the provider’s statement!
The Vault Admin Services Care Navigation team is there to help you find well-respected providers close to you to meet your needs. Mammograms, colonoscopies, MRIs, orthopedic procedures are all great examples of where Care Navigation can help you find the right provider. Call your Vault Admin Services team at 866-202-0029.
Your pharmacy benefits information will be on your benefits card. If you have specific questions about a particular prescription, call the pharma helpdesk at 833-464-9600. Have your card on-hand with your Bin and Group number.